Isabelle Bertrand, PT, PhD, CERAP/UFP
Cyril Dupuis, PT, MSc, CERAP/UFP
Christian Courraud, PT, PhD, CERAP/UFP

Introduction
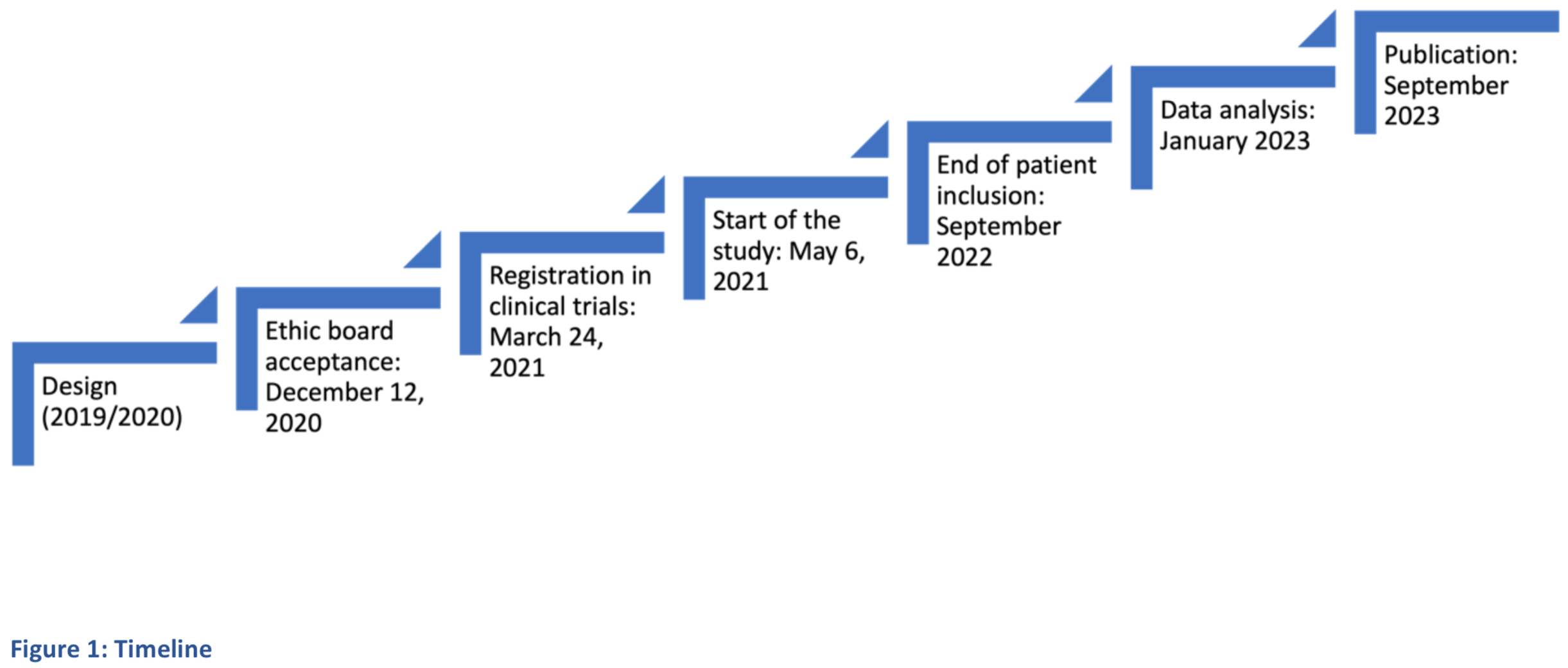
Implication of fascia in Low Back Pain (LBP) is probable [1-2], however, efficacy and specificities of fascial techniques remains to be shown and compared with other physical therapies [3-4]. This clinical study aims to evaluate efficacy of DBM Fasciatherapy on chronic LBP [5], combined or not with physiotherapy, compared to physiotherapy. Approval of the ethic board was delivered on December 2020. Inclusions started on May 2021 and should end in September 2022. Data analyses are expected in January 2023 (Figure 1).
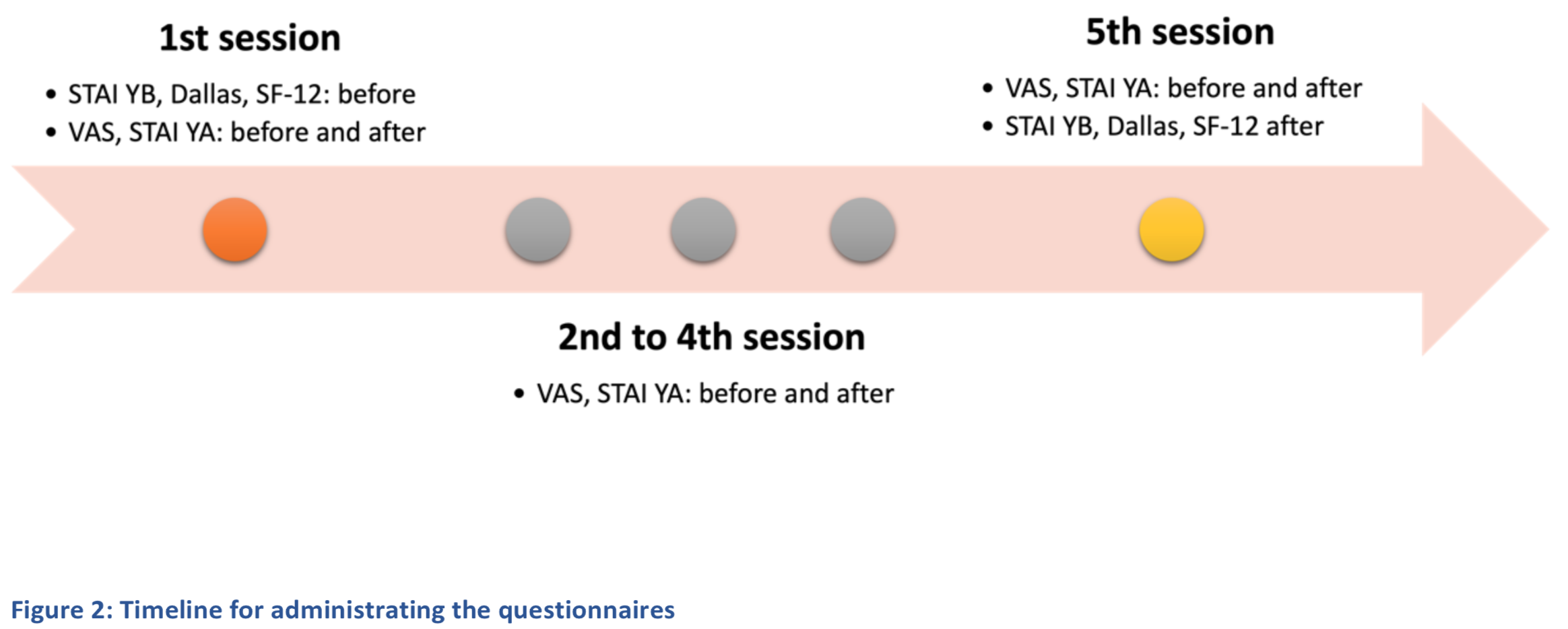
The primary outcome measure is pain intensity, measured with Visual Analogic Scale (VAS). Secondary outcomes are functional impairment (Dallas Pain Questionnaire), quality of life (SF-12), anxiety (STAI YA+B), medication consumption.
Practitioners must be physiotherapist trained in DBM Fasciatherapy (105 hours minimum). Patients must suffer from chronic nonspecific LBP, and to consult the practitioner for LBP for the first time.
The study has 3 arms: DBM Fasciatherapy, Physiotherapy, and Physiotherapy combined with DBM Fasciatherapy. Practitioners are randomized (design in cluster) by the statistical team. The expectations are 20 practitioners per arm, each practitioner following 3 to 5 patients for a total of 60 patients per arm.
The patient benefits from 5 sessions of 30 to 45 minutes, with an overall duration of 3 months. The questionnaires are submitted as shown on Figure 2.
Using questionnaires assessing several dimensions of LBP should give better insight on clinical relevance of DBM Fasciatherapy and how it can be combined with physiotherapy.
The limits of this study are related to methodological constraints needed by the study design (equate the groups, positives expectations from DBM Fasciatherapy, need for randomization, risking being out of usual practice for practitioners, difficulties to blind patients).
Conclusion
This study should give information useful for the reflection on complementary therapies, and their association with conventional approaches for LBP. The 3 arms should give insights on the efficacy of DBM Fasciatherapy compared to physiotherapy, and the relevance of combining the 2 approaches. The broadness of the dimensions of LBP evaluated should give details on this comparison.

